The Angelina Jolie Effect: The Public Impact of Celebrity Breast Cancer

A recent research study examined the impact of Angelina Jolie’s announcement related to breast cancer. In May of 2013, the actress announced she underwent a double mastectomy to reduce the risk of breast cancer, after testing positive for a BRCA1 gene mutation. According to this study, this announcement triggered a significant rise in the number of women with a family history of breast cancer being tested for the mutation, and this increase persisted for the next 5 months. The findings show that when it comes to health news starring a high profile celebrity, it can have a long lasting effect on the health of the general public. In the article, Evans adds that this encourages more women to visit family history clinics so they can find out about any gene mutations early and take the appropriate action. Although this will mean some women may need to have a mastectomy, he says that others may be advised to take cancer-preventing drugs or adopt lifestyle changes in order to reduce cancer risk, https://www.childinjuryfirm.com/strattera-atomoxetine. Both BRCA1 and BRCA2 gene mutations can be inherited from a parent, and they significantly increase the risk of breast and ovarian cancers, among others. Approximately 12% of women in the general population will develop breast cancer at some point in their lives, but around 55-65% of women with a BRCA1 gene mutation and 45% with a BRCA2 gene mutation will develop the disease. The researchers found that in June and July 2013—immediately after Jolie’s announcement—referrals for genetic testing increased two and one-half times compared with the same period in 2012, from 1,981 to 4,847. A 2-fold increase remained until October 2013, after which time genetic testing referrals began to fall. Angelina Jolie stating she has a BRCA1 mutation and going on to have a prophylactic (preventative) mastectomy is likely to have had a bigger impact than other celebrity announcements. This is possibly due to her glamorous image and relationship to Brad Pitt. This may have lessened patients’ fears about a loss of sexual identity following preventative surgery and encouraged those who had not previously engaged with health services to consider genetic testing. Many of the women seen at TurningPoint have increased family risk of breast and other cancers. TurningPoint cares for women who have had preventative breast cancer surgery in addition to those going through breast cancer. It is important for at-risk relatives to be aware of their family history and request screening or risk-reducing strategies. The Angelina Jolie effect; how high celebrity profile can have a major impact on provision of cancer related services. R. Evans, J. Barwell, D. Eccles, A. Collins. L Izatt. Breast Cancer Research 2014, 16:442
Exercise for Breast Cancer Survivors: How much is enough?

Early detection and improved treatments for breast cancer have resulted in better prognosis for patients. A recent review of research related to physical activity and breast cancer confirmed that exercise decreases risk of recurrence, increases quality of life, bone mineral density and strength and decreases fatigue and pain in breast cancer survivors. The study concluded that based on scientific data, breast cancer patients should be recommended to participate in rehabilitation programs including aerobic and strength training.(1) Many breast cancer survivors, however, are not sure how and when to proceed and ‘how much is enough’ exercise. The American College of Sports Medicine (ACSM) has exercise guidelines for cancer survivors.(2) The ACSM concluded that exercise training is safe during and after cancer treatments and results in many benefits for the patient. The amount of exercise recommended is 150 minutes of moderate exercise per week and 2 to 3 weekly strength training sessions of the major muscle groups. During the development of a physical activity program, it is important to consider pre-diagnosis fitness level, an understanding of the limitations that may be present due to surgical interventions and treatment of the cancer, and other medical conditions. A program should be tailored to a survivor’s needs, abilities, medical condition and interests. At TurningPoint, the physical therapists will evaluate each patient and their condition and create a program specifically to meet her needs. This can be monitored during treatment at TurningPoint and progressed as the patient regains more strength and flexibility. After discharge, appointments can be made for exercise consultation to review and advance the program as needed. TurningPoint also offers group fitness classes including Yoga and Pilates to help encourage flexibility and strengthening within a safe environment. Evigor S, Kanvilmaz S. Exercise in patients coping with breast cancer: An overview. World J Clin Oncol. August 2014, 10;5(3):406-11. Schmitz, Kathryn H. et al. American College of Sports Medicine Roundtable on Exercise Guidelines for Cancer Survivors. Med Sci Sports Exer. July 2010, 42;7:1409-1426
National and Regional Conferences Feature TurningPoint Experts
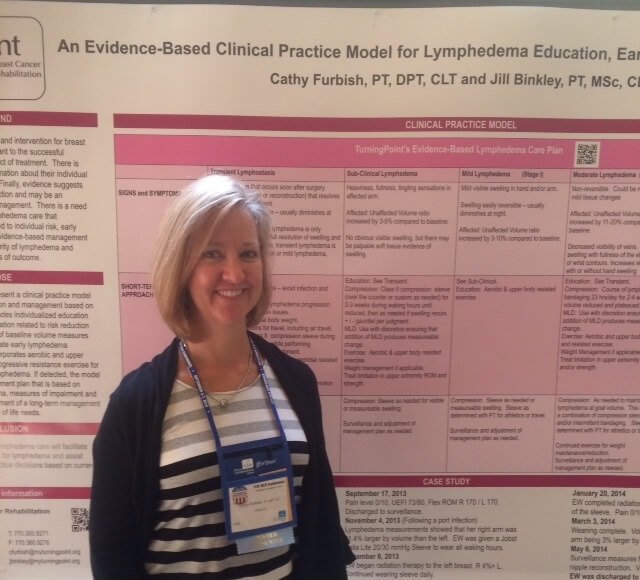
An important part of TurningPoint’s mission is to advocate for specialized rehabilitation care for all women with breast cancer. TurningPoint is heavily involved in educating the health care community locally and nationally about the role of rehabilitation and exercise for women with breast cancer. In September, Jill Binkley and Cathy Furbish, TurningPoint Physical Therapists, presented at the National Lymphedema Network’s International Conference in Washington, DC. Over 400 rehabilitation and healthcare professionals were at the conference. Jill presented the results of a collaborative research project between TurningPoint, the Avon Breast Center at Grady Memorial Hospital in Atlanta and Emory University. The intent of the project was to provide early rehabilitation intervention for underserved inner-city and minority women with breast cancer. Cathy presented TurningPoint’s model of evidence-based lymphedema care. The model includes early detection, patient education and, for women who develop lymphedema, a scientifically management strategy. Lauren Bober, TurningPoint Physical Therapist and Pilates Instructor, spoke at the Conference of Cancer Patient Navigators of Georgia about the Role of Physical Rehabilitation and Exercise for Cancer Patients. Lauren discussed early intervention, the benefits and importance of exercise for cancer survivors, the current recommendations for the frequency and duration and types of exercise for individuals with different types of cancers and gave recommendations on how to get patients involved with exercise.
Q&A with TurningPoint’s Jill Binkley on AJC.com

Sunday Conversation with … Jill Binkley 12:00 a.m. Saturday, Oct. 5, 2013 | Filed in: Local News A decade ago, Jill Binkley, a physical therapist, started TurningPoint Breast Cancer Rehabilitation, a nonprofit offering rehab services for women being treated for breast cancer. Binkley understood the enormous need for such services because she had undergone treatment for the disease herself. She also concluded that TurningPoint not only would focus on the physical side effects accompanying surgery, radiation and chemotherapy, but also would offer counseling, dietary and massage services. “I learned about and experienced many of the physical and emotional side effects of treatment that I was not aware of even though I was in the health care profession,” said Binkley, executive director of TurningPoint on Roswell Road in Atlanta. “That started me thinking, ‘Did other women have these issues as well?’” Many did and still do since one in eight women gets breast cancer, according to the American Cancer Society. October, which is breast cancer awareness month, is a time to celebrate advances in treating the disease. It also is a good time, Binkley says, to advocate for rehab services for the many women who suffer from the very treatments that save their lives. For more infirmation, go to myturningpoint.org. Q: What are specific physical side effects of breast cancer treatment? A: We often see pain in the shoulder and chest wall, reduced range of motion and difficulty with function such as reaching overhead, even lifting your baby. Lymphedema, which is swelling of the arm, is a chronic condition that affects about 20 percent of breast cancer patients. I am one of them. Q: What about emotional side effects? A: The biggest is the fear of dying and ongoing illness. Body image and sexuality follow, whether you have had reconstructive surgery or not. When you can help women feel better, that is a huge emotional boost. Q: You take a holistic approach to rehab? A: We try to take care of the whole woman. We have physical therapists. We also have a counselor, massage therapist and dietician on staff. Our clinicians work together in a comprehensive manner to help women through complex issues. Q: Has care for women improved since you were diagnosed? A: We absolutely have made some strides. When I got breast cancer, no one talked about the importance of exercise, which decreases the risk of a recurrence and is something we emphasize a lot at TurningPoint. The fact that doctors refer 30 new women a month to us means that they realize the importance of the care we provide. But, that is still just the tip of the iceberg. Q: Do other women just suffer silently? A: They don’t want to complain to the person who saved their lives. Just having a place like TurningPoint lets women know these side effects are typical and that it’s okay to seek help for them. Q: Why is your practice a nonprofit? A: We don’t turn any woman away. We do bill health insurance for our physical therapy services. We do get some large grants. If women need financial assistance, they get it. Q: Is working with breast cancer clients hard for you given your history? A: Whether you are a survivor or not, working with women with breast cancer has an amazing emotional impact on all of our staff in a very positive way. We get to know our women very well and that can be a very difficult because we lose some of them. The rewards definitely outweigh those very sad times. Q: Do you still worry about a recurrence 10 years later? A: The more minutes, the more days, the more months, the more years you live, the less chance you have of a recurrence and the less breast cancer is front and center of what you think every day. You can never say never. That is something you somehow learn to live with. The Sunday Conversation is edited for length and clarity. Writer Ann Hardie can be reached by email at [email protected]. Read the article online here.